7.Surgery for lymphedema: What is lymphaticovenular anastomosis?
In general, lymphedema is treated with conservative therapy (see the sixth column) and surgical treatment. Mild lymphedema, the cases in which degeneration of lymphatic vessels is less advanced (see the third column), can be treated with only conservative therapy. On the other hand, for the cases in which degeneration of lymphatic vessels is advanced and lymphedema has been exacerbated, the combination with conservative therapy and surgical treatment has been shown to alleviate symptoms of lymphedema, slow the speed of exacerbation, and reduce the incidence of cellulitis (infection).
This column explains "lymphaticovenular anastomosis (LVA)" that is the most minimally invasive technique among surgeries.
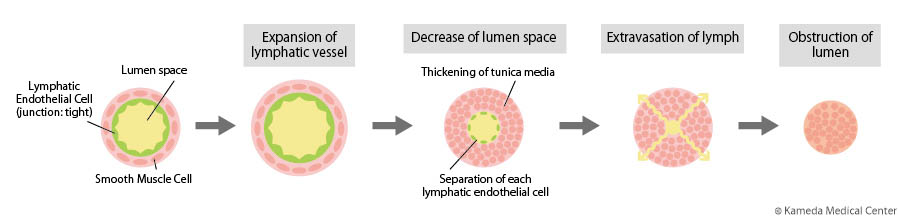
In treatment of cancers including breast cancer, uterus cancer, or ovarian cancer, if the lymph nodes are removed or radiotherapy is conducted, lymph flow in lymphatic vessels is stagnated, leading to degeneration of lymphatic vessels and progression of edema (see the second column).
Lymph fluid flowing from the hands and feet to the center of the body flows into the vein (right subclavian vein or left subclavian vein) at the "venous angle" near the heart, and returns to the circulation of body fluid (see the first column). However, because exacerbated lymphedema causes advanced degeneration of lymphatic vessels accompanied with stenosis or obstruction, lymph fluid cannot reach the venosus angle, and cannot join in the vein. Therefore, increased pressure inside lymphatic vessel and further advanced degeneration of lymphatic vessels result in a continuing vicious circle; that is, decreased recovery ability of lymph fluid in lymphatic vessel and exacerbated edema.
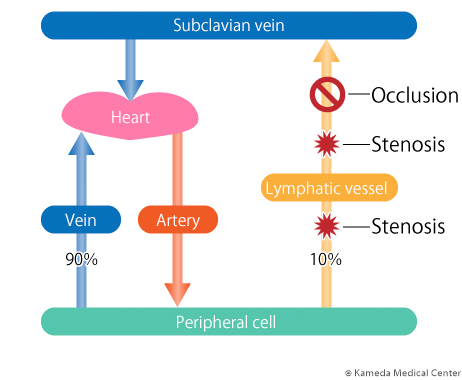
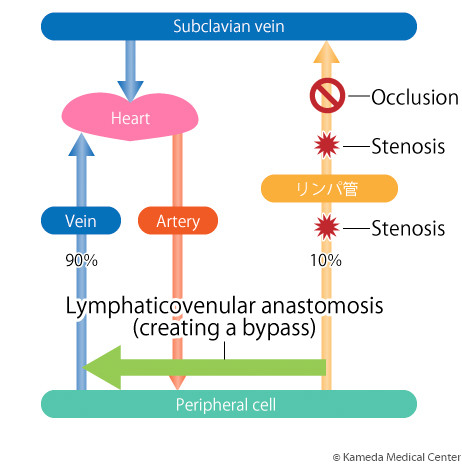
A major purpose of LVA is to stop this vicious circle. In the upper/lower extremities, the lymphatic vessel near the parts of stenosis or obstruction with less damage is chosen, and this vessel is connected to the vein to make "a bypass from the lymphatic vessel to the vein." As a result, stagnated lymph flow that cannot join in the vein is resolved, and degeneration of lymphatic vessel is stopped, leading to improved symptoms of edema.
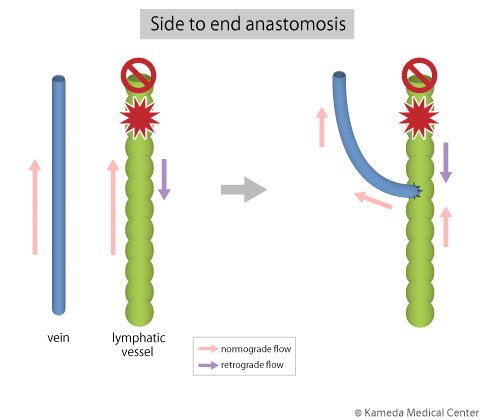
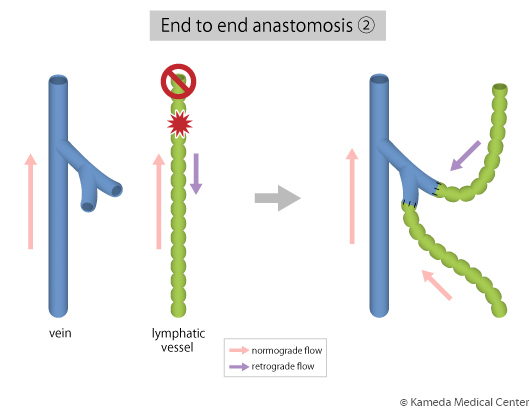
A primary feature of this surgery is that it can be minimally-invasively performed with less bleeding by little scar of about 2 to 3 cm in 2 to 5 sites (depending on severity) due to using a high-precision microscope. However, a major caution of this surgery is that an effect of it depends on condition of lymphatic vessels at that time. In other words, while the cases in which there are many lymphatic vessels with advanced degeneration and stenosis/obstruction have a lower effect of surgery, the cases in which there still are many lymphatic vessels with moderate or lower degeneration and lower stenosis have a high effect of surgery. Therefore, early diagnosis/treatment of lymphedema is important.

In our hospital, in order to maximize an effect of LVA with a smaller scar, patients are hospitalized on the day before surgery, appropriate lymphatic vessels/veins are identified using the current ultrasonography, and surgery is performed on the next day. The basic course is three-day/two-night stay (depending on patient'a desire, one-night stay or two-night or longer stay is possible), in which patients are discharged from our hospital after the effect of surgery is evaluated on the day after surgery. Patients can select the type of anesthesia (systematic (general?) anesthesia, conduction(?) anesthesia, local anesthesia) after the benefit and risk of each type are explained.